Procedures at our facility
Upper endoscopy enables the physician to look inside the esophagus, stomach, and duodenum (first part of the small intestine). The procedure might be used to discover the reason for swallowing difficulties, nausea, vomiting, reflux, bleeding, indigestion, abdominal pain, or chest pain. Upper endoscopy is also called EGD, which stands for esophagogastroduodenoscopy (eh-SAH-fuh-goh-GAS-troh-doo-AH-duh-NAH-skuh-pee).
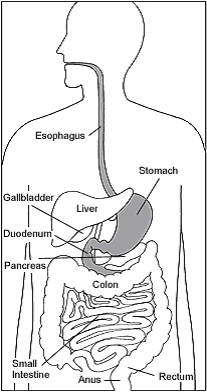 For the procedure you will swallow a thin, flexible, lighted tube called an endoscope (EN-doh-skope). You will receive medicine to help you relax during the exam. The endoscope transmits an image of the inside of the esophagus, stomach, and duodenum, so the physician can carefully examine the lining of these organs. The scope also blows air into the stomach; this expands the folds of tissue and makes it easier for the physician to examine the organs. This test does NOT exam the gallbladder or liver or pancreas.
For the procedure you will swallow a thin, flexible, lighted tube called an endoscope (EN-doh-skope). You will receive medicine to help you relax during the exam. The endoscope transmits an image of the inside of the esophagus, stomach, and duodenum, so the physician can carefully examine the lining of these organs. The scope also blows air into the stomach; this expands the folds of tissue and makes it easier for the physician to examine the organs. This test does NOT exam the gallbladder or liver or pancreas.
The physician can see abnormalities, like ulcers, cancers and inflammation, through the endoscope that don’t show up well on x rays. The physician can also insert instruments into the scope to treat bleeding abnormalities or remove samples of tissue (biopsy) for further tests.
Possible complications of upper endoscopy include bleeding and puncture of the stomach lining. However, such complications are rare. Most people will probably have nothing more than a mild sore throat after the procedure.
The procedure takes 5 to 10 minutes. Because you will be sedated, you will need to rest at the endoscopy facility for 30 minutes to one hour after your procedure. You may feel a little groggy after the procedure but most people feel very comfortable.
Colonoscopy (koh-luh-NAH-skuh-pee) lets the physician look inside your entire large intestine (another name for the colon), from the lowest part, the rectum, all the way up through the colon to the lower end of the small intestine, the terminal ileum.
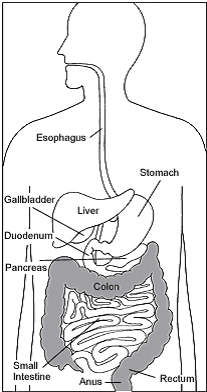 The procedure is mainly used to look for early signs of cancer in the colon and rectum. It is also used to diagnose the causes of unexplained changes in bowel habits, sources of bleeding, or in monitoring patient with inflammatory bowel disease, including Crohn’s disease or ulcerative colitis. Colonoscopy enables the physician to see inflamed tissue, abnormal growths, ulcers, and bleeding.
The procedure is mainly used to look for early signs of cancer in the colon and rectum. It is also used to diagnose the causes of unexplained changes in bowel habits, sources of bleeding, or in monitoring patient with inflammatory bowel disease, including Crohn’s disease or ulcerative colitis. Colonoscopy enables the physician to see inflamed tissue, abnormal growths, ulcers, and bleeding.
For the procedure, you will lie on your left side on the examining table. You will be given medication to keep you comfortable and to help you relax during the exam. Most patients sleep comfortably throughout the procedure. The physician will insert a long, flexible, lighted tube in to your rectum and slowly guide it in to your colon. The tube is called a colonoscope (koh-LON-oh-skope). The scope transmits an image of the inside of the colon, so the physician can carefully examine the lining of the colon. The scope bends, so the physician can move it around the curves of your colon.The scope also blows air in to your colon, which inflates the colon and helps the physician see better.
If anything abnormal is seen in your colon, like a polyp or inflamed tissue, the physician can remove all or part of it using tiny instruments passed through the scope. That tissue (biopsy) is then sent to a lab for testing. If there is bleeding in the colon, the physician can pass a laser, heater probe, or electrical probe, or can inject special medicines through the scope and use it to stop the bleeding. Bleeding and puncture of the colon are possible complications of colonoscopy. However, such complications are uncommon.
Colonoscopy takes 15 to 20 minutes. The medicine keeps you from feeling much discomfort during the exam. You will need to remain at the colonoscopy facility for 30 minutes to one hour after your procedure. You may feel a little groggy after the procedure but most people feel very comfortable.
Flexible sigmoidoscopy (SIG-moy-DAH-skuh-pee) enables the physician to look at the inside of the large intestine from the rectum through the last part of the colon, called the sigmoid or descending colon. Physicians may use the procedure to find the cause of diarrhea, abdominal pain, or constipation. They also use it to look for early signs of cancer in the descending colon and rectum and to monitor therapy in patients with inflammatory bowel disease including Crohn’s disease and ulcerative colitis.
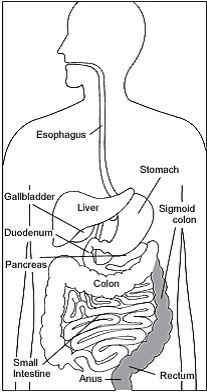 With flexible sigmoidoscopy, the physician can see bleeding, inflammation, abnormal growths, and ulcers in the descending colon and rectum. Flexible sigmoidoscopy is not sufficient to detect polyps or cancer in the ascending or transverse colon (two-thirds of the colon on the right side).
With flexible sigmoidoscopy, the physician can see bleeding, inflammation, abnormal growths, and ulcers in the descending colon and rectum. Flexible sigmoidoscopy is not sufficient to detect polyps or cancer in the ascending or transverse colon (two-thirds of the colon on the right side).
For the procedure, you will lie on your left side on the examining table. The physician will insert a short, flexible, lighted tube into your rectum and slowly guide it into your colon. The tube is called a sigmoidoscope (sig-MOY-duh-skope). The scope transmits an image of the inside of the rectum and colon, so the physician can carefully examine the lining of these organs. The scope also blows air into these organs, which inflates them and helps the physician see better.
If anything unusual is in your rectum or colon, like a polyp or inflamed tissue, the physician can remove a piece of it using instruments inserted into the scope. The physician will send that piece of tissue (biopsy) to the lab for testing.
Bleeding and puncture of the colon are possible complications of sigmoidoscopy. However, such complications are uncommon.
Flexible sigmoidoscopy takes 5 to 10 minutes. During the procedure, you may feel pressure and slight cramping in your lower abdomen. You will feel better afterward when the air leaves your colon.
The HET System is a new non-surgical device for the treatment of internal hemorrhoids. It is based on well-established scientific principles, gentle, simple and well-tolerated. The technology is cleared for use by FDA and European authorities. The hemorrhoids are treated with a unique ligation technology, resulting in their shrinkage and subsequent resolution of the disturbing symptoms. It is a gentle, simple technique and easy to use in the ambulatory setting.
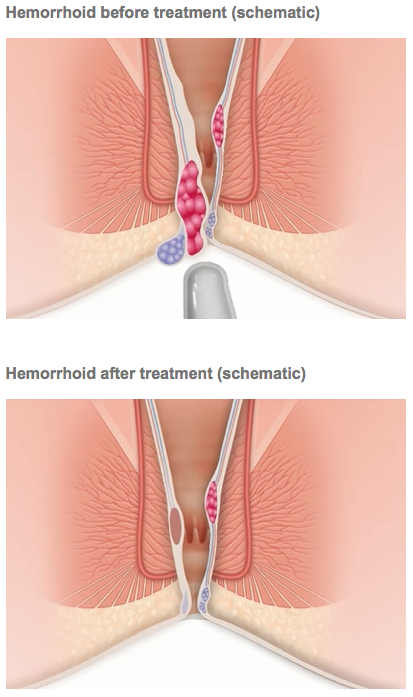 The procedure using the HET System is usually very well-tolerated and patients experience either no pain, or brief, mild discomfort. Typically, patients may return to work and normal activities right after the procedure.
The procedure using the HET System is usually very well-tolerated and patients experience either no pain, or brief, mild discomfort. Typically, patients may return to work and normal activities right after the procedure.
Typically, gastrointestinal bleeding is coming from a disrupted vessel in the mucosa or submucosa of the stomach or intestine. The bleeding can present itself as a bright red blood in the stomach or rectum or dark discoloration of the stool. The blood might also not be visible with the naked eye, and should be diagnosed by a clinician using blood count and analysis of the stool specimen. The cause of the bleeding can be fairly innocent or very serious. It is important, therefore, for the physician to accurately diagnose and visualize, whenever possible, the bleeding location using endoscopy or other established techniques.
The most common cause of a rectal bleeding is the bleeding from internal hemorrhoids due to significant straining (constipation, heavy lifting, chronic coughing, difficulty with urination, etc.) and aging. Hemorrhoids frequently enlarge during pregnancy due to increasing pelvic pressure applied by the growing fetus. Painful hemorrhoids typically develop after vaginal births, but usually resolve without intervention within 2-4 weeks after delivery.